Evan Rosa: For the Life of the World is a production of the Yale Center for Faith and Culture. For more information, visit faith.yale.edu .
[Music]
Lydia Dugdale: I've had patients who've looked at me and said, "I have no idea what I believe, and I'm scared out of my mind; I'm dying." And what's the doctor to say to patients then? So I started thinking about this and came across this body of literature, the ars moriendi, and what struck me about the ars moriendi-- in Latin, "art of dying"-- is that it developed in the aftermath of the bubonic plague outbreak that struck Western Europe in the mid 1300s. And really it was a pastoral response, if you will, to the concerns of the laity--the lay people--who said, "look, our priests are dying, or they're skipping town. There's no one to perform burials or last rites. And for all we know this can be damning to our souls. We need some help to prepare for death."
Evan Rosa: This is For the Life of the World, a podcast about seeking and living a life worthy of our humanity.
Drew Collins: Dylan Thomas is perhaps most famous for his poem "Do not go gentle into that good night". The first stanza, which reads,
"Do not go gentle into that good night / Old age should burn and rave at the close of day;/ Rage, rage against the dying of the light."
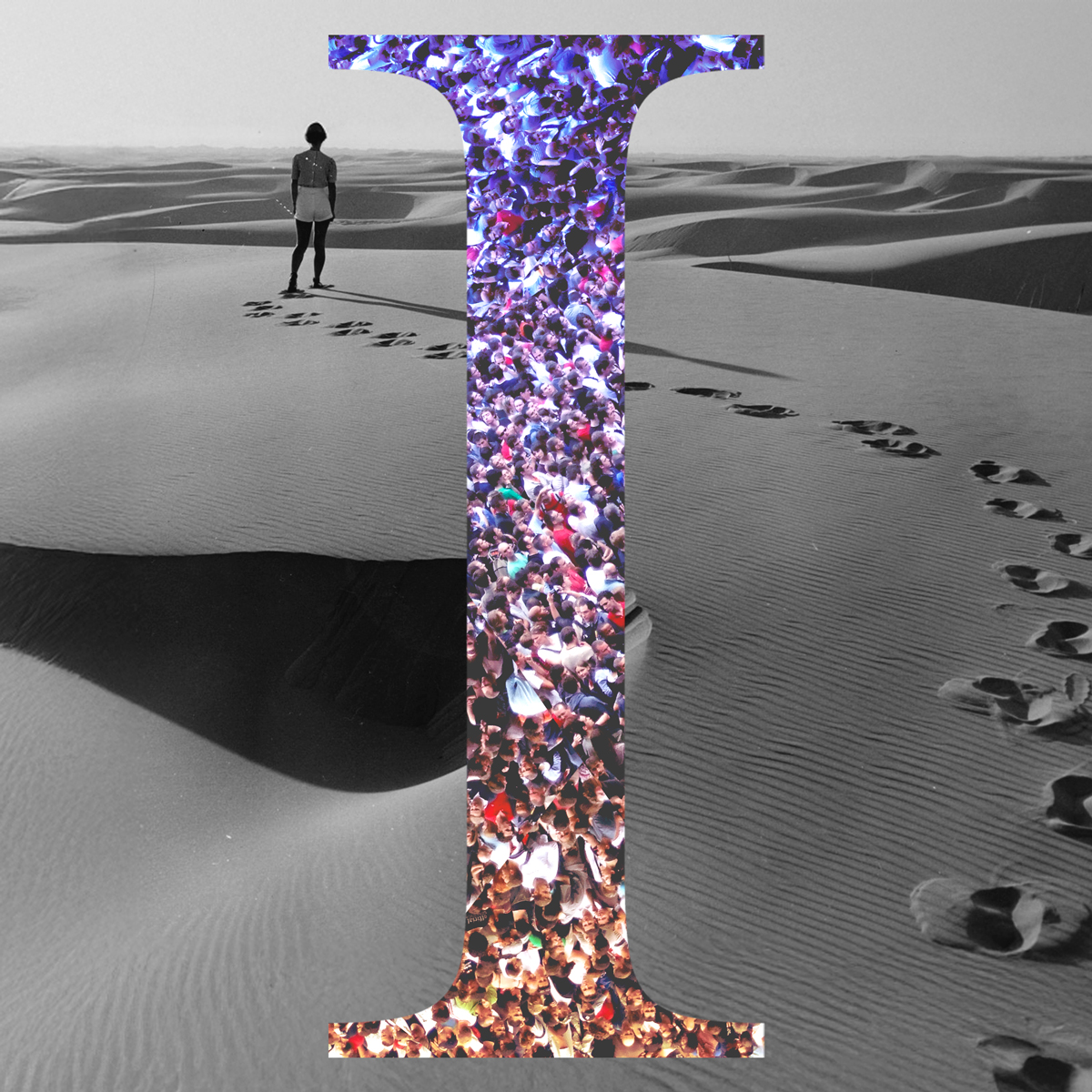
I'm guessing most of us can identify with this feeling. It feels intuitively, if not objectively, true; we tend to think death-- the dying of the light--is the enemy of life or at least the enemy of a good life, and rightly so. But what if, at least on this side of God's kingdom, dying well is an important part of living well?
If we're not prepared to ask questions about what it means to die well, lingering with Thomas in stubborn and rage-filled opposition to death's very reality, will we ever be prepared to ask questions about what it means to live well?
I'm Drew Collins at the Yale Center for Faith and Culture. Today we're joined by Dr. Lydia Dugdale, associate professor of medicine and director of the Center for Clinical Medical Ethics at Columbia University. She's an internal medicine primary care doctor, a medical ethicist, and is author of "The Lost Art of Dying: Reviving Forgotten Wisdom" forthcoming from Harper Collins this summer.
It's a book about a mostly forgotten ethical tradition and text that emerged in response to the black plague and late Middle Ages, ars moriendi-- that's Latin for "the art of dying." And to say that this book is timely is probably an understatement. In this conversation, Lydia and I talk about what it's like right now to be a doctor in New York city, the epicenter of the pandemic in the U.S. and maybe the world.
The importance of focusing not just on health, but also flourishing and that very human side of sickness and death. She explains the tradition of ars moriendi, "the art of dying," and offers insight and guidance on the meaning of death in the context of a meaningful life.
[Music]
Lydia, I know it's not under great circumstances, but I'm really grateful for this opportunity to check in with you again.
Lydia Dugdale: Thanks, Drew. It's great to be here with you.
Drew Collins: And I really just wanted to start off by saying that you've been on the front lines of fighting this pandemic in the sort of epicenter in the United States and, I suppose, in the world.
And so I just want to say thank you for all that you're doing.
Lydia Dugdale: My pleasure.
Drew Collins: And I wanted to start off by just getting a sense from you of how this is different, how you're treating and relating to covid patients, those were sick and dying. And how does that feel different from your normal medical practice?
Lydia Dugdale: Sure, Drew; As you know I'm relatively new to New York city, just having moved here about nine months ago, so I did not yet have a patient practice established in New York. In contrast to typical business-as-usual medical practice, I don't know the patients who are walking through the door. And, in fact, there have been so many patients who've come to the hospital recently, many of whom are not even patients that are typically coming to our hospital or to our medical practices. So many of them are new to the healthcare system, which means every face is a new face; we don't necessarily have any medical history on many of these patients, and we're sort of starting from scratch with each person.
Now, the ones who are able to have a conversation, and we're able to assess what their needs are and get them taken care of, they often go home. But the ones that are coming into the hospital are the ones who typically are really too sick to talk much. They're having such difficulty breathing; their oxygen levels are so low.
These are patients that, not only do we not know them, even from the medical charts, but we can't really get to know them. And so one of the common refrains that I've heard from many doctors is that what's different right now is that we are essentially managing very sick people without the opportunity to get to know them or their families. Because in most hospitals right now families are not welcome, visitors are not welcome, because of concern of spreading the virus.
In addition to that, because it's so contagious, healthcare professionals are trying to limit their exposure to individual patients. And so we are largely monitoring from computer screens and computer monitors that are sort of measuring vital signs, blood pressure, oxygen levels, et cetera.
So we're really missing out on that human connection. And I think that is what has caused some of the most distress is people are very sick and we don't know who they are, and we're really taking care of them in isolation from their communities and their histories and their stories and all of that stuff that makes them human and gives us that social relationship; we just don't have that right now.
Drew Collins: It's easy to imagine what sort of the negative impacts that would have on a patient. An added layer of complexity to that is that a lot of these patients are also perhaps intubated or medically induced comas.
Lydia Dugdale: Yea, that's right, or frankly, just having a lot of difficulty breathing. Patients are profoundly fatigued, so they're so tired. I can wake up some patients and talk to them, but they quickly are ready to recline again and rest, and they don't have a lot of oxygen to spare. It's just difficult to have conversations all around, whether they're intubated or not, whether they're in the ICU or not.
Drew Collins: So my question is what impact does that dynamic have on medical professions and health care providers?
Lydia Dugdale: The language that a lot of people are using right now is the language of moral injury, which comes from the military literature--this extreme distress, even feelings of guilt and anguish and doubt that come from treating in these sort of wartime conditions. And I don't want to overstate things; it's been very difficult in New York. There's some of the hospitals have been hit much harder than other hospitals. On the whole, I think what we have faced is far less severe than we had anticipated.
So even just sheer numbers are far lower than we had thought we would be facing, which is good because most hospitals have been able to significantly increase their capacity and, frankly, haven't been maxed out. We have not, for example, faced the kinds of shortages with mechanical ventilators and things like that that we were anticipating.
But when you're working really hard to save people's lives, but they aren't really human in the way that we usually think of doctors relating to patients--and I don't want to suggest that the doctors are dehumanizing the patients--the situation is so dehumanizing:
patients can't talk; they're out of breath; they're exhausted; they're intubated. And we're supposed to spend as little time with them as possible. This is in contrast to a typical day in the ICU or the intensive care unit in a pre-covid era, where families would be at the bedside. We have, you know, family waiting rooms.
The doctors would routinely meet with families almost every day to give updates. So even if we can't talk to the patient who is intubated or have a meaningful interaction with that patient, we still get to know who they are as human beings from the context of their families. And that is is absolutely missing right now.
So a lot of distress all around.
Drew Collins: You mentioned moral injury. I was wondering if you could just say a little bit more about that, explain what it is for some listeners who aren't familiar.
Lydia Dugdale: Well, I'm certainly not an expert on it, but as I mentioned it's a phrase that comes from the combat veteran literature.
It's a phrase that the military will use frequently. People --soldiers in particular-- on the frontlines, enduring such difficult circumstances in battle...and maybe being forced to do things that that cuts against the core of who they are and who they understand themselves to be.
An example might be having to open fire in into a situation where you know that the person who's targeted is there, but there will be collateral lives lost--children may die, expectant mothers may die, things like that. And then what some soldiers will describe as just such intense feelings of shame and guilt because what they had to do for the sake of the mission--and, perhaps, one could say saving the most lives overall--meant that they had to do things that they wouldn't have even chosen to do, but they just had to do it because of the circumstances. And those feelings of, of shame and guilt can lead to some pretty profound dissonance within oneself, prompting the sort of questions like, who have I become? What am I doing?
And in the military literature, at any rate, they distinguish this from PTSD or post traumatic stress disorder in several nuanced ways. This is kind of a deeper, prolonged internal sense of shame and guilt. And so, it may not be fair to use that language in medicine right now. Certainly having several really, really bad weeks in New York is not the same as months of being engaged in a kind of dehumanizing fight.
At the same time, it may be too early to tell what the impact is going to be on healthcare professionals. I know there are people actively studying this, trying to figure out just how much this is going to affect people long-term. And then there are all the other issues of morale, right?: shortages of staff, concerns and fears about having enough protective equipment, anxiety about what happens when we resuscitate patients that we know will definitely not benefit, but we're doing it because families insists on it. But at great peril to ourselves because the act of resuscitation sends virus all over the place. And so there's just a lot of fear and anxiety right now and on all levels.
Yeah, and so I guess whether moral injury is absolutely the appropriate term remains to be seen. But that certainly is a phrase that keeps popping up right now in discussions.
Drew Collins: It's helpful getting a framework of what the impacts are on healthcare providers, not just on the victims of the virus themselves.
Lydia Dugdale: That's right. And I just want to say, quickly, that it's not just doctors and nurses. I mean people have been operating the subway system and the buses in New York city just to get folks to the hospital, right? Huge numbers of them are getting sick and food providers and maintenance crews and folks cleaning the hospital.
Many of these individuals are already living right at the brink of economic peril. And if they get sick or they lose someone who's a breadwinner, the impact can be absolutely devastating. I feel like there's all this heroism around doctors and nurses and, you know, there's a point to that. But there are so many involved in the care of patients right now and many very much unsung heroes. I think it's worth just mentioning that, putting that out there. It's a huge team, absolutely huge team.
Drew Collins: Yeah, that's a good point. Point taken. So wondering if we could speak about this in a slightly more personal tones, if you're okay with that.
I just was wondering if you might share what sort of worries or fears you have personally about this pandemic. What are you most fearful or worried about?
Lydia Dugdale: With regard to how the virus is playing out in New York City, there have been many people have died, as you know, and that is a huge tragedy for so many people here. But there are a lot of hidden costs and hidden concerns that trouble me and maybe trouble me more than the lives lost from the virus.
As tragic as that is, and I do not wish to go on record as minimizing that data; it's absolutely devastating. And there've been weeks where the ambulances in New York city are non-stop, or the other day, the EMS broken through a window of an apartment on my street, I think because someone had died and they were trying to get the body out.
It's pretty in your face here. There are 40-some odd tractor trailers that have been deployed that are refrigerated around the city; they're essentially a portable morgues. So it's not like it's not in your face; it really is in your face. But there are a lot of other things that we aren't giving as much attention to, like the children who are not in school right now. I've talked to New York city public school teachers who are working in districts that are struggling and they say their goal is just to connect by telephone with all of their kids once a day.
This is not instruction. These kids are going to lose out on a half of year or more of instruction. And these are children who already are coming from difficult circumstances. There's a number of children who depend on public schools for their meals, right? One of the reasons that there was a big struggle over shutting down the schools here is because we have children who are going hungry because they were dependent on school to eat.
And, of course, the economic toll. One of the things that I've loved in my short time of living in New York city is how lively all of the storefronts are. And walking down the same streets now, so many small businesses were already operating at the brink of loss, and they have just shuttered.
They shuttered because if you say to them, you know, you have to close your doors for a month, these are people who cannot afford to close doors for a month. And so they've just shut their businesses. They just took the loss. And I'm not a particularly anxious person, but I think I have spent a considerable amount of time thinking about how do we make sense of the health effects of this economic downturn? So not thinking economy versus lives lost now, but the bigger picture, the macro way we think about human flourishing. People are not flourishing right now; children are not flourishing; victims of domestic violence are not flourishing right now.
And the longterm consequences just remain to be seen. I think about that a lot, and I think about it really in terms of health and flourishing and not economics versus saving lives.
Drew Collins: I wonder if, using language that I'm drawing from you and from your recent book, if the distinction might also be framed in terms of fears or responses to avoid death at all costs versus those that seek to uphold and provide the possibility of dying well.
Lydia Dugdale: I know it's not a very popular view right now to say why are we throwing all of our resources into fighting off deaths when really it would be better to anticipate our mortality and prepare for it. That's not a very popular view. And yet my work and my forthcoming book, I think bear this out.
On some level, we've deceived ourselves into thinking that we can escape our mortality. The last hundred years in the U.S., medicine has become so powerful and so successful that we really haven't had to spend much time thinking about our finitude.
And yet in an earlier era--pretty much any time leading up to the last hundred years--whether it was famine or plague, some sort of pestilence or war, every few years something was ravaging a population. People lived with this sense of precarity. They were so much more precarious than we live now, and so maybe this current moment will help us reorient our. Attention to our finitude and then motivate us to think about what really matters. How we want to reset and restructure our lives, to work toward that which matters most, how we even think about these big questions of meaning and purpose, these questions of human existence.
So I'm hopeful that this will change that conversation. But it certainly is difficult to even talk about that right now when really the dominant theme is doing everything we can to save one life, which, again, is a laudable goal. I'm not disparaging that, but doing everything we can to save one life...
And, there's not been much conversation at all about the need to actually prepare well for our deaths.
Drew Collins: Mm. Right. So let's talk more about this, because you've got a book coming out this summer called "The Lost Art of Dying: Reviving Forgotten Wisdom". I know this is a sensitive subject right now, but if I understand you correctly, we've fallen into this situation where we're having a debate right now about whether or not about the relative merits of saving lives versus economic concerns and considerations.
And what you're saying is that another way of framing this conversation about medical interventions and how we save lives is thinking about not just avoiding death and the cost of avoiding death, but what kind of death we need to also embrace.
Lydia Dugdale: That's right. Maybe embracing is overstating it just a bit.
Drew Collins: Yeah, fair enough.
Lydia Dugdale: It's actually one of the big criticisms of this body of literature that I write about this ars moriendi, which is Latin for "the art of dying". One of the big critiques of it is that it does commend to death. I don't know that any of us really wants to commend death. Death still casts an enormous blow on a family and a community, right?
I mean, this language of the sting of death is completely accurate. Death rips holes in people's lives. So we don't want to commend it. At the same time, it's inevitable, right? Mortality has always been a hundred percent, so it's going to happen and then we can meet death prepared or ill-prepared, and that decision is really up to us and our communities.
Drew Collins: How did you get interested in this?
Lydia Dugdale: Oh, goodness. I grew up in a household where the talk of death was pretty common. My grandfather had been a bomber pilot in World War II, and he had had a plane malfunction at one point and crashed. His flight instructor was beheaded in the crash.
My grandfather was hospitalized for months, and then he was supposed to have an honorable discharge, but he wanted to go back in. And they let him go back in and then he was shot down during World War II. He was a prisoner of war. So the man had nine lives.
And we, he talked about death all the time and was on fantastic terms with his undertaker. He bought cemetery plots for himself and my grandmother, right after the war, actually; it was one of his first items of business was to make sure that if they died, the things were worked out.
He had written his funeral years in advance. But he was also this very funny guy. So it would all be done. It would all be talked about in this kind of light-hearted manner. But the tone under it all is death is a fact of life. And so you might as well get your stuff in order.
So I grew up in that kind of an environment, and it wasn't really a scary thing. But then when I ended up in medicine, and the trainees, the residents in medicine, really bear the brunt of some of the longest hours. And I would spend hours with patients in the intensive care unit.
And they many times died these sorts of horrific deaths that cause great distress to everyone--the patients, their families, the caregivers, the doctors, the nurses. We were all just so distressed.
And then I took care of patients who were in those situations but recovered and said to me, "Dr. Dugdale. I never, never want to be back like that again. I don't care what it takes. I'm not going back to the intensive care unit like that again." And so there's a way in which I witnessed so much highly medicalized dying, and yet people were unprepared for it. Not only these sort of concrete decisions--
Do I have CPR? Do I undergo cardiopulmonary resuscitation? Do I go to the intensive care? Do I get the mechanical ventilator, get intubated?-- but also bigger questions. I've had patients who've looked at me and said, "I have no idea what I believe, and I'm scared out of my mind. I'm dying." And what's the doctor to say to patients then, especially when the patients are actively dying and they suddenly realize they're dying and they have no idea what they believe.
So I started thinking about this and came across this body of literature, the ars moriendi, and what struck me about the ars moriendi-- Latin "art of dying"-- is that it developed in the aftermath of the bubonic plague outbreak that's struck Western Europe in the mid-1300s and really it was a pastoral response, if you will, to the concerns of the laity--the lay people-- who said, "look, our priests are dying, or they're skipping town. There's no one to perform burials or last rites. For all we know, this can be damning to our souls. We need some help to prepare for death."
And it took a while for the church to get its act together. This was a time in history when the church split. There were two men claiming to be Popes, and then, later, three men claimed that they were the legitimate Popes.
So there's all this fracturing, and I'm not a Catholic historian so take it for what it's worth. But at any rate, when the church finally got attacked together in the council of Constance in the early 1400s. One of the first, responses was to address this concern of the masses.
Basically, how do we prepare well for death? Life is too precarious. We need help. And so when I stumbled across this and I thought, Oh my goodness, this is incredible because this is empowering patients to think about their finitude in the context of community. To wrestle with these big life questions and to do it now, while they are at whatever age they are but before the end.
One of the great things about the ars moriendi is it sort of prescribed sayings, kind of a Q&A, like a catechism. There were prayers, there were instructions, but this was given to all members of the community, so that even if you were a little kid and at the deathbed of a dying elder, you too could participate in this care of the dying and in so doing, in reciting these questions and answers or these prayers, you were already starting to rehearse for your own mortality. It was brilliant. And this went on over the course of the lifetime. And you know, I told you it sort of grew out of the Catholic church, sort of pre-Reformation Catholic church.
But by the time of the Reformation, the Protestants picked it up; Jeremy Taylor did a version, and by the 1800s it, of course, came to the U.S., spread all over Europe--lots of languages. But the versions that ended up coming to the U.S. some were religious, but some were completely secular.
So if you were brought up well, anticipating and preparing for death was just part of it. You know, it's just part of what it meant to be raised well. Now we might have estate planning, you know, people who've come from families of means will talk about estate planning. Well, you know, 200 years ago they just talked about how have you made your peace? Have you figured this out? Do you know how you will die? And not so much the circumstances, but where are you at big picture with these big questions?
And so what I loved about this is it really put the project in the hands of everyone. It wasn't tied to a particular religious denomination or even a particular religion. And these are the tasks of a lifetime or in order to die while you've got to live well.
Drew Collins: Hmm. That's fascinating. I want to pick up on what you just said: what does the art of dying well tell us about how to live well?
Lydia Dugdale: In the book, I make the case that if there's so much that it could mean, but if it meant nothing else, it would be a constant acknowledgement of, or awareness of one's finitude.
That is carried out within the context of a community that helps people--that individual--makes sense of these big life questions. So that that would be the kind of lowest common denominator--living well in order to die. Well, because then you're working out your answers to these questions within the context of a supportive community of like-minded individuals who are also thinking about these questions with a view to the end game, right?
And that's why I think that's the lowest, most basic level of an "art of dying." And I think that's something that is achievable for most people today, no matter what your particular affiliations. I was on a call with some students talking about this stuff, and one of the students explained to me how she identifies and said, "I may not be able to talk to my family about this, but I identify with this particular community and they do help me make sense of these questions."
So, if in earlier times, these were very much questions of family. I think now, given the mobility of society and the ways different things matter, people are finding different communities where they can wrestle with these questions; but I think that's the lowest bar.
But there's so much more to say about that: how can these communities help us address fear of death? How do we acknowledge fear? How do we hold our palms open to the possibility of having fear of death and saying that that's okay, yet not running from death itself. To that end, I actually rely in my book on some of the writing of Christian Wiman, who writes very beautifully about the fear of death.
And then there's more, there are different ways we can also think about this: what are the rituals that are important for anticipating death, for grieving immediate loss, for addressing grief in a more protracted way? I mean, all of this stuff has been worked out in various traditions and worked out very beautifully and deeply enriched me.
So the work has been done, and I often tell people, "you don't need to invent this, but you should tap into what's been done and interrogate it." I mean, certainly there are questions of spirituality, right? There are religious answers to some of these ultimate questions, questions of meaning and purpose, like what happens when I die? Where do I go?
That would be an additional layer, a sort of a deeper layer of working out the art of dying the ars moriendi so some of these other themes I think are all part of it.
Drew Collins: I guess from your perspective death is a part of life and so an absence of and understanding of death means an absence of an understanding of life.
Lydia Dugdale: Yeah, that's right. There's a way in which the thought of death or the threat of death brings into relief that which we most value. And so if we aren't living with a view to that sort of end game, we're really missing out on making sense of how we should use our time. Which relationships we should invest in, how we should spend our money, what we should give away.
You know, I mean, all of all of these questions: do we live in isolation or not? How do we think about pride? How do we think about individual gain versus community good? Having sort of a view to our death can help us make sense of all of those questions.
Drew Collins: That's helpful; I want to actually turn to some sort of practical questions there, and I was wondering if you could just speak a little bit more about the practical dimension of the ars moriendi: what sort of practices or things do we need to anticipate in order to imagine what a good death would look like and to carry it out?
Lydia Dugdale: The reason why the answer to that question is a little bit trickier is because it would depend in part on the communities that help us make sense of our answers. But I think that there's a way in which even an introduction of the conversation goes so far in helping us work toward identifying practices. So for example, we're in the midst of this coronavirus pandemic. I'm living in a relatively small apartment--well, relatively nice apartment but small by the world's standards, certainly-- with my family in New York City. My children are distance learning; my spouse is working from home; I'm working from home when I'm not in the hospital. We're not supposed to spend much time in public space. At the beginning of this, a month ago, it was pretty hard on all of us.
We weren't used to spending this much time together. We're all introverts, and we were all getting on one another's nerves and there just was really no place to hide. And we all needed devices to do our thing. But we started talking about that as a family. And my kids are little--they're eight and ten--so they're certainly not adults.
And we started talking about this as a family. We started talking about the numbers in New York City. We looked at the maps together. We talked about how many people were sick and how many were dying. We talked about the articles in the newspaper about young people under the age of 50 who were dying.
And we talked about how that meant that there was no guarantee that mommy and daddy would get to the other end of this and we would all be together.
And so our conversations started shifting then to, "okay, well how do we want to live together? How do we want to treasure our days together? How do we want to express gratitude together? Because we can choose to see this time as a real drag and, frankly, for the parents who are trying to hold down jobs, as an impediment to being as effective and as efficient as we would like to be." Or we can say, "this is a unique season for us to invest in our relationships and figure out what really matters to us and to work toward that together."
And so those were helpful early conversations, but it took at the very beginning and acknowledgement of our finitude. We had to be willing to have those tricky conversations with little kids from the beginning.
And especially when I first started going into the hospital, knowing that I was going to just be coughed all over and come home and total germ factory, it felt like a bigger conversation to have. And I'm somebody, you know, who loves talking about this stuff, and I've spent a long time talking about this stuff.
Drew Collins: So we've talked a lot about how living well is an important factor in dying well, and one thing in particular that seems important is community; we need to live and to confront our own mortality in community with others. But that's precisely the challenge today for those who are sick and dying, and not just covid patients but anyone who's dying under shelter-in-place orders, quarantines, or isolation.
Lydia Dugdale: Yeah, you're right that there are some real challenges today.
There have been a lot of initiatives to try to contact patients who we suspect wouldn't do well in the hospital with covid before they come to the hospital. So I'm aware of groups of oncologists, cancer doctors, for example, who are calling all of their patients and having frank conversations about the experience of covid in the hospital and what to expect. Because we want patients to be informed that they will end up dying alone if they really succumb to this illness.
And, of course, we know that these folks with underlying severe diseases are much more likely to die from it. And we want them to know that dying alone may be a real possibility. And so I'm aware of groups of palliative care doctors also who are doing similar things with the patients that they follow, but sort of trying to get the messaging out that right now dying in the hospital from covid does mean dying apart from family.
For the most part, I think some hospitals are making very few exceptions, but of course, I can't speak for particular hospitals. It's a real problem right now, and it's a source of a lot of sadness. It's very difficult for the healthcare workers on the front lines who are really the ones holding the iPads or the iPhones to do FaceTime with family members as patients are dying. And then, of course, as we talked about earlier, it's so difficult if a patient is quite short of breath to even be able to have a conversation. So, you know, the relational piece is really being challenged right now.
Drew Collins: So, I want to know, can we die well if we die alone?
Lydia Dugdale: You know, I wouldn't say that dying alone is the same as lonely dying. And that's a distinction that I make in the book. Many people--especially people who throughout the course of their lives, hated to be a burden on others-- will often hang on until all the family members have gone home for the night. This is in a non-covid time, and I've seen this so many times. So characteristically sort of classically, it's the people who just don't like to be a bother to anyone, so those people then are effectively dying alone, but the dying process has not been a lonely one. So that distinction is important.
And then I think taking sort of a step back and saying, what does it mean to die well? And part of what we've been talking about is the importance of working out one's answers to these big questions, right? So the person who dies surrounded by family and friends but with a deep sense of discontent about things, isn't dying a lonely death and isn't dying alone, but perhaps, may be experiencing a sense of, of disconnectedness that that is something kind of deeper and more difficult to describe. And that's what I'd like to see people work toward--exploring the answers to some of those deeper questions.
So that's all part of what it means to die well. So yeah, real challenges today in the present moment, but not insurmountable if one is sort of attended to the tasks of preparing to die well over the course of a lifetime.
Drew Collins: Lydia, thank you so much for spending time with us today. I can't think of a more important and timely conversation than this.
Thank you for this, and thank you so much for all the work you're doing in hospitals and with other healthcare professionals.
Lydia Dugdale: Thanks so much, Drew.
Drew Collins: We're living under a cloud of death or at least the threat of it right now; I'm used to clouds, living in new England. But the thing about clouds is that when you notice them mostly for what they hide, that brilliant blue of the sky, the warmth and light of the sun, maybe death is like that too--something that we tend to think about mostly in terms of what it hides, what it interrupts, what it ends.
Perhaps death like clouds is meaningful to us only insofar as it gets in the way of those things we deem good about life. That just as clouds are a part of the earth sky, not just interruptions on it, so to is death a part of life. And as such, I'm grateful for Lydia's efforts, both as a physician who cares about human dignity in the face of death and as a guide of a tradition of living and dying well. Thanks for listening, friends, we'll be back with more next week.
Evan Rosa: For the Life of the World is a production of the Yale Center for Faith and Culture at Yale Divinity School. This episode featured Drew Collins interviewing Dr. Lydia Dugdale, New York city physician and associate professor of medicine and director of the Center for Clinical Medical Ethics at Columbia University.
I'm Evan Rosa and I edited and produced the show. For more information, visit us online at faith.Yale.edu, and for a new show every Saturday and sometimes a mid-week, subscribe to the show. You can find it on any mobile podcast app, and if you're enjoying the show, we'd be grateful for your support. The best way to support us in these early stages is to share and review: something as simple as telling a friend, posting on social media, and leaving a rating and review in Apple Podcasts.
Thank you for listening, friends. We'll be back next week.